You may be thinking, "Wait, self-treat my back pain... isn't that your job?" As a physical therapist I often work with people that have low back pain. It shouldn't be any surprise, as it affects around two thirds or more of residents of the United States. The fact of the matter is, our current health care system does not empower people with the knowledge that they need to take action at the first onset of low back pain. Most people don't even know who to see first. If I may get on a very small soapbox for just a moment... very small... physical therapy should always be the first choice of practitioner in treating low back pain. Yes, even before your primary care physician, even before you get an X-ray or an MRI, and even before Chiropractic. Direct access laws allow this and that is their purpose; to avoid needing a referral first. But even BEFORE physical therapy, you should have the tools needed to at least do something for yourself when it first happens. My job is not done if you are not empowered with the knowledge to help yourself. For the next 11 weeks I will be writing a post just like this one sharing some of that knowledge with you about the steps that YOU can take to self-treat low back pain. That is the intent of this series. To skip the steps below and watch the video, please click here.
Injury prevention is something that is discussed often in the physical therapy world. Many physical therapists that work with athletes focus on this area, whether its running, or soccer, or golf, etc. Perhaps more uncommon is the idea of injury that can take place for musicians, specifically when playing a keyboard instrument such as the piano or organ. One might wonder how an injury might occur just sitting on a bench playing the piano, but in reality there are multiple ways that injury can occur while playing the piano or organ. Recently a close friend of the family who is a music teacher and who offers piano lessons brought this topic up and wrote her own blog post about this very topic. I will be the first to admit that I had never considered this in the past. Please be sure to read her post here, as I was featured as a guest on her blog. She asked some great questions about this topic and I was able to give some expert advice. In my post I would first like to highlight some of the possible injuries that can occur, as well as to provide a list of ten exercises that one could do for prevention. These would serve as a warm up prior to sitting at the bench in order to prevent injury through proper posture and adequate flexibility. So, what injuries are possible while playing a keyboard instrument? First, the wrist/hand and forearms are a potential source of problems due to development of carpal tunnel syndrome (CTS), ligament sprains at the wrist/digits, and even neural tension at the wrist, elbow, or shoulder (or all three) due to poor posture. Posture is a crucial aspect of injury prevention. Ideally, one should be sitting upright with feet flat on the floor (unless using pedal with right foot or playing pedals on an organ), shoulders back, and head erect with eyes relaxed looking at the keys/sheet music. The hands and wrist should be relaxed, as if sitting on top of a bubble. If this is NOT done and the individual is slouched, multiple impairments can result. Namely: shortened and tight neck muscles (can result in tension headache and compression of cervical nerve roots), increased strain of upper back and shoulder muscles (results in poor shoulder stability and lack of support for the neck), increased stress on the discs and facet joints of the lumbar spine (ligament strain of the joints of the back and possible disc bulge or rupture), shortened and tight hip flexor muscles (also results in more stress on lumbar spinal segments), etc, etc. The take away here is that posture is HUGE for preventing injuries at the piano/organ. What can be done about this, besides maintaining adequate posture? The exercises I am about to recommend will go a long way to facilitate good posture while playing, flexibility of the neck, upper limbs, and trunk, as well as to promote warming up the tissues prior to playing. Let's face it, playing a musical instrument can by physically challenging and can certainly be a form of exercising. For piano, the hands must be limber and agile to play each key and to reach octaves, etc. And if the song is a fast tempo and has a large range of notes, the entire upper limb system is getting a workout. My hands and arms are always fatigued after a long session at the piano. This is expected and perfectly natural. So, as before any workout, a warm up is essential. And no, I don't mean sitting at the piano and cracking your knuckles and your neck. Leave that for the cartoons. The last part of this post will be to highlight the exercises that will provide a well rounded warm up for injury prevention. There is a video linked to this post to see the exercises in action and then a written list below the video. Recommended Exercise Routine The following exercises are found in the video that you just saw above. If you are looking for an exercise ball and yoga mat like used in the video you can get them via the links in this post. * For the following exercises, I recommend 5-10 repetitions of each immediately prior to sitting down on the piano bench. *As an Amazon Associate I earn from qualifying purchases
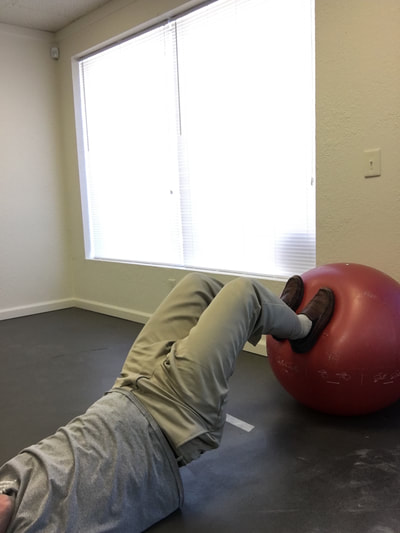
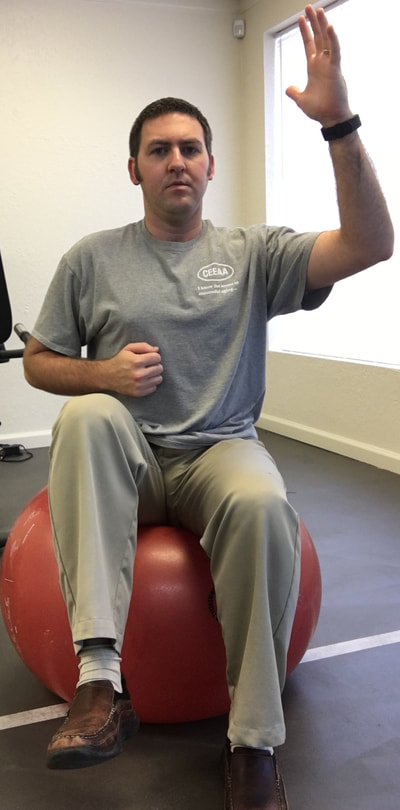
1. Standing pectoralis doorway stretch - This will help to open up the chest, stretch the pectoralis muscles, and to encourage erect posture. 2. Standing pectoralis/biceps stretch - Again, this encourages opening up the chest and bringing the shoulders and arms back. Tightness in pectoralis major and minor can result in neural tension of the brachial plexus (this is the bundle of nerves that exit the neck, under the collar bone, and into the shoulder and arm). 3. Standing upper limb prayer stretch/neural glide - This exercise moves the entire upper limb through a range of motion that encourages lengthening the nerves of the upper body through all of the bends in the limb. This is not as specific, but is a great warm up exercise. 4. Median nerve glide - This is a specific stretch for the median nerve of the upper limb. This is the culprit in carpal tunnel syndrome as the median nerve is often compressed at the wrist. 5. Radial nerve glide - Another specific stretch for the radial nerve. This supplies the sensation for the back of your hands and is the motor nerve for the muscles that extend the fingers and wrist. 6. Ulnar nerve glide - A specific stretch for the ulnar nerve. This supplies the sensation for the half of the palm near the ring and pinky fingers. This nerve can be compressed at the elbow (where your funny bone is) as well as at the wrist (Guyon's tunnel). Guitarists may need to worry about this one more than the medial nerve, but both are important to stretch for the keyboardist. 7. Cervical/neck rotation, side bending, and flexion/extension - These are combined due to the fact that they are all the same area of the spine. These are great for general flexibility for the joints of the neck while turning the head right and left, bending to the side, and looking up/down. This is important for limbering up the joints of the neck as well as warming up the muscles that will be working to hold your head up while playing. 8. Standing trunk rotation - General flexibility exercise for the upper and lower back to loosen up the joints of the spine and warm up the muscles of the trunk 9. Back extension - General flexibility exercise for the lumbar spine to encourage good sitting posture and to move the spine in the opposite direction of slouching. This can alleviate soreness in the back as well. 10. Lower trunk rotation with legs on ball - Good general flexibility exercise for the lower back muscles and joints. This can be a great one for relieving stiffness and soreness in the lower back as well. If you are looking for an exercise ball you can purchase one here.* *As an Amazon Associate I earn from qualifying purchases In this case, I mean in the LITERAL sense! So, here's the thing, there are a TON of exercises that you can do with an exercise ball.* If you have worked with me as a client before, or if you plan to in the future, there are so many ways you can prescribe exercise, even a home exercise program, with a ball* such as this. Why? Well, they are light weight, relatively easy to store, and you can do so many exercises without even using weights and you will really get a workout! I thought I would put together a list of exercises that would be really useful if you obtain a therapy ball. Any of the links found in this post will take you to a ball that I recommend in particular*. The GoFit professional stability ball is the one that I use in the clinic and in my videos, because its not expensive and it even comes with printed exercises on the side to give you an extra challenge and ideas of what to do. WARNING, I would NOT start with the ones printed on the side of this particular ball. But I am going to give you even MORE ideas so you can get started now! ( Wave your mouse over images for caption). These particular exercises would be helpful for back pain. *As an Amazon Associate I earn from qualifying purchases So here goes: Prone Glut Sets Bridges on ball Lower abdominal sets Ball crunches I hope you find these exercises helpful and that this gives you an idea of how you might manage back pain by obtaining a therapy ball. This one tool could save you lots of time and money due to space savings and versatility. For more information, please call me today to discuss other ideas for treating your back pain. 918-251-7199.
P.S. If you are looking for a soft spot to lay this yoga mat is the one I use and I love it because of its extra cushioning! Be empowered! *As an Amazon Associate I earn from qualifying purchases 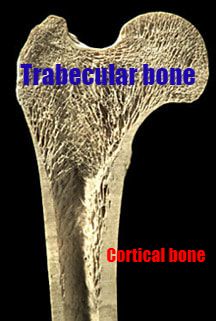 Image courtesy of ASBMR Educational Materials https://goo.gl/images/NR4gxM Image courtesy of ASBMR Educational Materials https://goo.gl/images/NR4gxM Osteoporosis (OP) is a condition effecting the bones and is associated with very low bone mineral density (BMD). The name itself means "porous bones" and results in the bones becoming brittle and leading to fractures due to bone fragility. This is typically associated with women, but men can also have the condition as sex hormones diminish over the decades. Most, if not all people with OP, started out with osteopenia (low BMD, but not yet progressed to osteoporosis). This is the best time to prevent onset of OP, but even those with OP can prevent worsening of the condition, prevent fractures, and prevent falls that lead to fractures. Osteoporosis Canada has great resources on the condition. The full list of "fast facts" can be found here, but to me one of the most profound listed is that 80% of fractures in those 50+ are due to OP. Many of these folks will not be diagnosed with OP and will not be prescribed the correct preventative treatment. Medications and supplements are very important, but exercise is a crucial medicine for OP. Why Exercise Is Important With OP Reason 1: Preserving bone density. With aging we all start to lose bone density as young as our thirties. The amount of exercise and physical activity that you challenge your body with, as well as the amount of calcium that you consume in youth, have a direct impact upon the health of your bones as you age. Think of it as a bank where you make deposits over time. The more you store up for the future, the more healthy your bones are. But again, why is exercise so important? Two words: Wolff's Law. Wolff's Law states that bone will adapt to the stresses placed upon it. The more stress, the more the bone will grow. The lower the stress, the less bone will grow. The bone that is particularly susceptible to becoming brittle and fracturing is called trabecular bone, or cancellous bone. Let's look at the anatomy for a moment. Trabeculae are bony projections within the bone that result in a matrix or lattice work that supports load bearing. The long bones of the body such as the humerus and femur have trabecular bone in the ends where the load is particularly important, for example the shoulder and hip. The vertebrae of the spine also contain trabecular bone. While the cortex of the bone, the outer wall, is also thick in the ends of long bones due to load bearing, trabeculae provide even more support for tension or compression forces in the bone. Think of them as little columns or buttresses supporting the large outer walls. These structures are the first to go with OP and literally make the trabecular bone disappear. Without this extra support fragility fractures are highly likely. Weight bearing activity and resistance training places stress upon the bone and results in bone building that can protect from losing bone density over time. Even if you already have OP when you start exercising, these types of exercises will still help to prevent fractures. Reason 2: Preventing Falls As we age our muscle tissue will slowly deteriorate if nothing is done to prevent it. Last week, we discussed sarcopenia, or progressive muscle tissue loss, as a preventable disease of advanced age. Preserving muscle strength is not only important for bone health, as the bone at the musculotendinous junction is thickened by the pull of muscle placed upon it, but also just as important for preventing onset of weakness in the lower body and trunk. This weakness results in poor balance reactions to prevent falls and inability to stop fall once a loss of balance occurs. Falls are a source of many of the fractures that occur with OP. Remember the statisic we saw earlier about 80% of fractures in the aging adult being the result of OP? If we can prevent the falls that lead to the fractures through exercise we can also prevent the loss of bone mineral density that leads to OP at the same time. 1 in 4 adults over the age of 65 will fall in 2018. How many will break a hip or a wrist, even a vertebrae? How many will not return home after they fall? Our easy chairs are more deadly than most people realize. It's time to get moving! What Exercises Are Safe with Osteoporosis? As a physical therapist, exercise prescription is a daily part of my job. With aging adults this takes more skill and adaptation. There are many ways to strengthen the muscles and to preserve flexibility without stressing the spine in a dangerous way. This is where a PT is so valuable and why we need to be training more people that are not therapists in exercise programs that encourage bone health without danger of fractures. There are programs out there that are very valuable that I will provide links to below. The guidelines of the ACSM state the following for recommendation of exercise for people with OP: Frequency: Weight bearing aerobics 3-5x/wk (if not daily) and resistance training 2-3 days per week Intensity: For aerobics, moderate exercise starting at 40% and working up to 60-80% of heart rate reserve. For resistance training, moderate intensity at 10-13 on Borg Rating of Perceived Exertion and 60-80% of 1 rep maximum. Time: 30-60 minutes total each day of exercise Type: Weight bearing aerobics such as walking, jogging, or elliptical. Water aerobics also valuable. Resistance training with bands, weight machines, or anti-gravity with supervision of a physical therapist. Here is what to look out for ->
At Hyland Physical Therapy and Wellness we are developing an exercise class for people with osteoporosis that is based upon the guidelines we have discussed today. This would be available in group format, but at any point I am available to consult with you individually to develop a safe program specifically for you. Contact me today to find out more. The links below will help you to get in touch with me. |
AuthorDr. Michael Hyland, DPT, CEEAA has been a physical therapist since 2012. He is a Certified Exercise Expert for the Aging Adult and an expert in Parkinson's Disease. He owns Hyland Physical Therapy and Wellness in Broken Arrow, OK Archives
October 2022
Categories
All
|
Proudly powered by Weebly











 RSS Feed
RSS Feed